Endovascular Treatment for Osteoarthritis
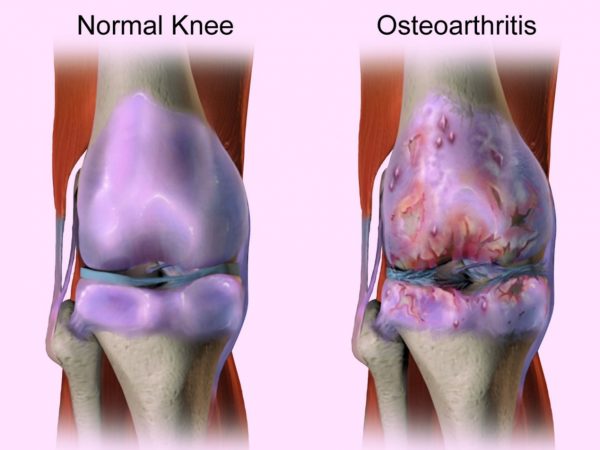
What is Osteoarthritis?
The most common type of joint inflammation that affects the quality of life of millions of people worldwide.
Osteoarthritis is caused by the erosion of the articular cartilage and may affect any joint in the body, although the most common joints are the knees, thighs, hands and spine.
The erosion of the cartilage causes joint narrowing and direct friction between the bones which results in pain and sometimes joint distortion.
What are the common symptoms?
- Pain – mainly during movement of the joint
- Stiffness – difficulty moving the joint mainly after sleeping or prolonged inactivity
- Tenderness when touched
- Swelling
- Loss of flexibility
Risk Factors:
- Age
- Gender – women tend to complain more of this condition
- Obesity
- Congenital illnesses – metabolic/osseous
- Injuries
There are many treatment methods available, topical ointments, specific physical activity, injections to the joint, and even joint replacement surgery if the condition is irreversible.
The common opinion today is that the active disease is accompanied by a local inflammatory lesion, that causes the abovementioned symptoms.
A new currently accepted treatment method, is embolization of the arteries that feed the inflamed area, designed to decrease blood flow to the afflicted area and to restrain the inflammatory reaction.
There are many advantages to this method over surgery:
- Quick recovery and resuming normal activity
- Painless procedure
- Avoiding anesthesia
- Low complication rate
- Locating the specific blood vessels that feed the inflammatory area and preserving the normal blood vessels
Who is a suitable candidate for this procedure?
Candidates for embolization are patients that have chronic osteoarthritis who do not feel improvement with conservative treatment and present symptoms that do not improve by medication and do not wish or cannot undergo invasive surgical procedures. The candidates must have reasonable renal function.
How is the procedure performed?
The patient, lying down, is monitored for pulse, blood pressure and oxygen levels. The procedure is performed by an interventional radiologist after local anesthesia, usually in the groin area. Mild relaxation medication may also be administered. The doctor will then make a tiny incision and through it insert a thin tube (catheter) to the artery and maneuver it to the treatment site. A small amount of contrast agent is injected for the radiologist to properly view, by imaging, the arteries that supply blood to the afflicted area and locate where to apply embolization (close them).
The surgeon then emits tiny particles that cause an obstruction of the indicated arteries.
By obstructing the arteries, the blood supply to the afflicted area is reduced and it will subsequently decrease the inflammatory lesion. At the end of the procedure, the catheter is removed and pressure is applied to the incision area. There are no visible sutures, the incision is covered with a dressing. This procedure is usually completed within 2 hours.
What is the recovery process?
After the embolization, the patient is discharged the same day of surgery, and may resume normal activity within several days. Improvement of pain level is expected several hours after surgery due to the reduction of the inflammatory lesion.